Entry 11
Written October 25
Pre-surgery Appointment
Pre-surgery Appointment
So far, so good. My prostatectomy is scheduled for about a month from now. We'll discover the exact time this week.
It does help to have someone with you when you visit the specialist because more questions and answers tend to be generated. I went solo to today's pre-surgery information appointment with Dr. Saranchuk, the urologist/surgeon and his resident. My note-taker, Margaret has accompanied me to many of my previous appointments but she's in Vancouver with her elderly mother for a couple of weeks.
By comparison to past appointments, this one was brief, less than half an hour. It hadn't been necessary to feed the parking machine for three hours.
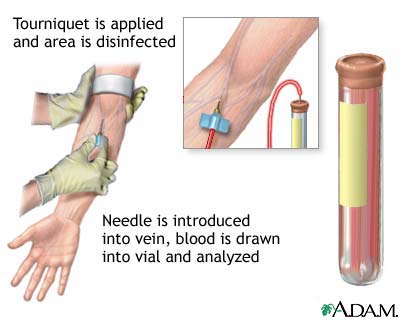
During our meeting, the urologist explained the surgical process and the potential side effects once more. One new thing I learned is that there will be some blood loss during the surgery. In anticipation of that, my own blood will be drawn and stored just before the surgery. Other fluids are added to compensate for the drawn blood. He also told me that the average hospital stay is three days.
He reassured me that he would be doing the operation. We were wondering about that as this doctor is also an assistant professor working for a faculty of medicine in a teaching hospital.
Now, the wait......
During our meeting, the urologist explained the surgical process and the potential side effects once more. One new thing I learned is that there will be some blood loss during the surgery. In anticipation of that, my own blood will be drawn and stored just before the surgery. Other fluids are added to compensate for the drawn blood. He also told me that the average hospital stay is three days.
He reassured me that he would be doing the operation. We were wondering about that as this doctor is also an assistant professor working for a faculty of medicine in a teaching hospital.
Now, the wait......